
Table of Contents
- What Is PDA?
- History, Origins & Debate About PDA
- PDA and Autism
- What PDA Looks Like Day-to-Day
- Why Demand Avoidance Happens
- Assessment, Prevalence & Impact
- Support Strategies for PDA
- Frequently Asked Questions
- Conclusion & Next Steps
In Focus
- PDA is a demand-avoidant profile marked by intense anxiety around everyday expectations.
- It is most commonly described within the autism spectrum but is not officially recognised in the DSM or ICD.
- PDA behaviours often stem from anxiety, sensory overload, and a strong need for autonomy and control.
- Early recognition helps families, teachers, and clinicians offer appropriate support and reduce conflict.
Pathological Demand Avoidance (PDA) is a demand-avoidant profile often associated with autism, characterised by an intense need to resist ordinary demands and maintain control. This guide explains what PDA stands for, how the PDA profile differs from typical demand avoidance, and why it remains a debated but meaningful concept within autism research and neurodivergent communities. AuDHD Psychiatry is a neurodevelopmental assessment and diagnostic clinic trusted by individuals and families across the UK, offering clarity on complex profiles like PDA.
If you recognise PDA traits in yourself or a family member, you can book a free introductory call to explore whether an autism or ADHD assessment might help.
What Is PDA? (Definition & Core Traits)
Understanding What PDA Stands For
Pathological demand avoidance refers to the prevalent drive to resist acting upon everyday demands made by other people, or even by regular responsibilities. It may be widely recognised as a behavioural profile of autistic individuals, often referred to as “PDA profile,” but it’s important to understand that it’s not a formal diagnostic category. It’s a pattern where you avoid following expectations, along with feeling distress when facing them. If you’re an individual who has autism, this profile gives you an explanation of why seemingly simple tasks can cause extreme or intense emotional reactions.
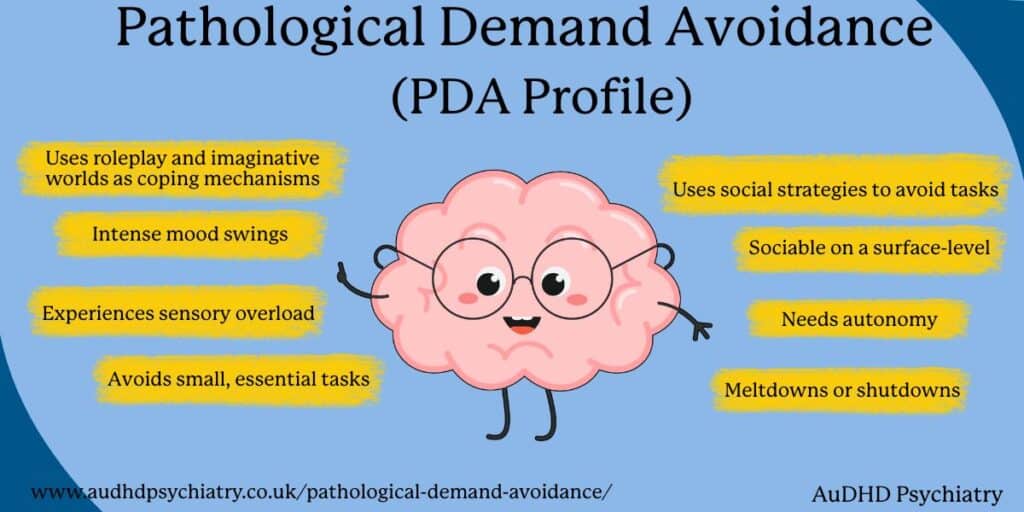
The Core Features of the PDA Profile
If you’ve ever used social strategies to manage or escape expectations (this can be through humour, distraction, negotiation, playing a role, or pretending not to hear), you might have done it to protect yourself from anxiety or overwhelm. This behaviour is one of the defining features of PDA, and it’s also why it may be misunderstood as an individual being manipulative, rather than self-regulation.
Another trait that’s common to a PDA profile is the strong need for autonomy and control. When this happens, demands don’t only feel inconvenient; they also feel like a threat to you. You’ll feel an intense need to keep your autonomy and control, which may result in avoidance and mood changes. This can result to simple, essential tasks like brushing your teeth or going to school or work to feel like a burden and trigger high levels of stress.
Role Play, Imagination, and Emotional Regulation
Many people with a PDA profile use role play and imaginative worlds as coping mechanisms. These immersive roles provide distance from real-world pressures and can reduce anxiety. However, shifting back into everyday demands can be difficult, resulting in shutdowns, panic, or sudden emotional shifts.
As we’ve previously mentioned, if you have a PDA profile, you may want to use role play and imaginative worlds as coping mechanisms. Getting into these roles can be immersive and give you a break from the pressures caused by the real world, and can therefore reduce your anxiety. Doing so can make switching back to reality and working on your responsibilities extra difficult, so much so that it can result in shutdowns, panics, or sudden emotional shifts.
PDA also overlaps with emotional dysregulation, particularly when demands accumulate or feel unavoidable. This can make it more challenging to regulate, which is one reason why being aware of this experience is important.
PDA vs Typical Demand Avoidance
Not every person avoiding everyday demands are experiencing PDA. Typical demand avoidance is part of everyday life. Most people delay tasks, negotiate responsibilities, or avoid stressful commitments. PDA, however, involves a pervasive and extreme response, driven by anxiety rather than preference. The avoidance is automatic, intense, and rooted in a nervous system that perceives demands as threats.

History, Origins & Debate About PDA
Where Pathological Demand Avoidance Began
Pathological demand avoidance syndrome was first used by the British psychologist Elizabeth Newson in the early 1980s when she recognised a cluster of children whose avoidance behaviours, social strategies, and anxiety-driven behaviours did not appear to fit the traditional presentation of autism. Newson characterised this cluster as pathological demand avoidance syndrome, considering this to be part of a pervasive developmental disorder.
Newson’s works became the pillar of the PDA profile, and autism advocates and support groups in the United Kingdom began receiving and employing the idea.
Why PDA Sparked Intense Debate
Despite PDA being accepted and recognised by a majority of clinicians, educators, and families, PDA remains excluded from the DSM-5 and the ICD-11, the internationally accepted primary diagnostic texts for mental disorders, which sparked debate. Some argue that PDA represents a profile of autism in a class of its own, a behaviorally determined class of autism, or simply the presentation of traits and characteristics of autism in conjunction with a significant degree of anxiety.
This controversy is recognised in The PDA Society and The National Autistic Society, and, within the United Kingdom, the level of advocacy and support varies, with some clinicians and researchers using the profile in clinical practice, while many others dismiss the concept as a loose or informal description rather than a reliable category of autism.
Global Variation and Cultural Debate
PDA is most commonly recognised in the United Kingdom, with comparatively much less in other countries, including the United States and Australia. There is very little research regarding PDA, with a lack of large-scale studies, and no agreement regarding what the condition is and where it resides within the autism spectrum disorder. There is a consensus in systematic reviews that more research is needed to ascertain the disorder’s origins, its neurobiological correlates, and what forms of assistance would be most beneficial.
The Growing Role of Community Knowledge
The condition is unrecognised in official discourse, and so most of what is currently understood has come from the autistic community, including adults, members with PDA, family members, and community organisations. These individuals have provided the experiential knowledge that has enabled the development of language to identify behaviours that have been neglected, and thus have developed support systems.
PDA and Autism
How PDA Fits Within Autism Spectrum Disorder
Even if PDA is not an officially recognised diagnostic subtype, a number of specialists and scholars have deemed it as a potential profile of autism spectrum disorder. It is centred on a particular grouping of characteristics—extreme demand avoidance, social strategising, excessive anxiety and a pronounced craving for independence. These attributes are also seen in autistic individuals, but in a different configuration, particularly in highly demanding and unpredictable situations, an outlier.

PDA in Autistic Children and Autistic Adults
Autistic children with traits of PDA tend to approach normal requests with negotiation, diversion, laughter, and other emotional alterations. These are not characterised as intentional defiance, but they’re a display of distress. Adults potentially have a differing presentation, characterised by social withdrawal, internalised avoidance, and demand shutdowns.
The anxiety from a perceived loss of control can make authority figures more complex of a challenge, as it silences control and can exacerbate anxiety to trigger avoidance. PDA children and adults commonly experience difficulty with transitions, school routines, work tasks, or any scenario that can trigger feelings of pressure.
PDA-Like Traits in Non-Autistic Children
Some children who are not autistic present with patterns that may be PDA-like, linked with anxiety disorders, trauma responses, or, sensory overwhelm. This leads to frequent misdiagnoses with, e.g., oppositional defiant disorder or conduct disorder, even though the emotional drivers are different.
Both parents and clinicians may find it difficult to separate demand avoidance that is anxiety-rooted, and anger or rule-breaking defiance. Understanding the individual’s nervous system and emotional profile is essential for accurate interpretation.
The Relationship Between PDA, ADHD, and Late Recognition
PDA often co-occurs with ADHD. This includes emotional dysregulation, problems with executive functioning, and engagement with tasks in a non-steady manner. Because of this feature overlap, a lot of people, especially adults, remain undiagnosed for long periods of time.
If your child or family member shows patterns of extreme demand avoidance and you’re unsure where to begin, speaking with a specialist can provide clarity. At AuDHD Psychiatry, our clinicians understand PDA-like profiles, autistic presentations, and anxiety-driven behaviours. You can book a free introductory call to explore your concerns and discuss next steps:
What PDA Looks Like Day-to-Day
Core Characteristics of PDA in Everyday Life
Most autistic people with a profile of PDA will find that their daily life is dominated by a persistent and extreme need to avoid all forms of demand, whether verbal or non-verbal. This might involve getting dressed, starting on school or homework, participation in a family activity, or simply responding to a question. Whereas to some degree, every child and adult will show a need for resistance from time to time, with PDA symptoms involving automatic, extreme, and anxiety-driven pushback or demand avoidance that becomes so disruptive to daily life and functioning.
Surface Sociability and Social Communication Strategies
Surface-level social communication remains an astonishing facet of PDA. With it, you might look and sound quite socially confident. Social articulation may seem effortless. You might even appear socially and psychologically charming.
However, you may also notice that people with this sociability tend to less psychologically engaged. Sociability may thus engage less transactional communication to escape or mitigate some demand. As previously mentioned, this may include social strategies of humour, distraction, negotiation, social avoidance, or unresponsiveness.
Some people tend to externally express their distress through visible behaviours, like negotiation loops, meltdowns, or abrupt shifts of affect. Others may internalise, privately withdrawing, freezing, or masking their anxiety until they collapse. Whether you belong to the first group or the latter, neither demonstrates deliberate avoidance, as these scenarios reflect a neurodivergent nervous system under strain.

Role Play, Imagination, and Emotional Regulation
As you try to provide yourself with flexibility from everyday demands of life, you may engage in another common feature of PDA: role play. For some autistic individuals who are more socially-engaged, this is a typical self-protective coping mechanism. It isolates the individual from emotionally stressful demands.
However, switching back to reality, such as in school or doing household routines, stopping this protective coping response may induce spikes in anxiety or cognitive dysregulation.
Why Demand Avoidance Happens
The Anxiety-Based Foundations of PDA
Pathological Demand Avoidance stems from extreme anxiety. Routine expectations can bring on a stress response, change the body and activate the sympathetic nervous system, and bring on a sense of threat. A request can be something as simple as talking to a person or putting shoes on, yet PDA can make it feel unmanageable.
In individuals with autism, intolerance of uncertainty magnifies the stress response to a task. When a task is perceived as controlled, and the person feels overwhelmed, they implement a protective mechanism by avoiding the task.
Sensory Overload and Emotional Lability
Sensory overload is a common phenomenon in the PDA population. Things like strong lighting and noise or sudden changes in the environment can cause the nervous system to undergo a state of dysregulation that makes the environment feel even more threatening. Mood dysregulation, or emotional lability, can also occur and tends to happen more frequently when the nervous system is already low in resources.
Demand avoidance intensifies when there is an authority figure instilling expectations or when there is a sense of rigidity or unpredictability in the environment. For many PDA children and adults, such demands signal the potential loss of control over their way of functioning. From an emotional safety standpoint, it is essential to maintain autonomy over the situation, and thus, avoidance of the demands becomes the primary coping mechanism.
The Primary Function of Demand Avoidance
Despite its challenges, demand avoidance often serves a necessary function:
- Self-protection from distress
- Emotional regulation in overwhelming environments
- Reducing perceived threat
- Maintaining autonomy when control feels uncertain
Understanding this reframes PDA not as wilful behaviour but as a nervous-system-driven response.
Assessment, Prevalence & Impact
How PDA Is Identified in Clinical and Everyday Settings
As PDA is not officially recognised in clinical settings, taking into account the home, school, and social environments, practitioners seek to document patterns. Observations show that there is often a high degree of anxiety, avoidance coping, transitional difficulties, and distress around expectations. A behavioural profile, not a diagnostic label, serves to inform the understanding of the demand avoidance patterns.
The DSM-5 and ICD-11 don’t include PDA as a standalone condition. Instead, the behaviours that include demand avoidance are regarded as part of the broader autism spectrum disorder profiles. Thus, there is a high degree of variability in clinical practice. Some clinicians consider PDA to be an identifiable separate profile while others consider it to be a mix of autism, anxiety, and emotional dysregulation.
Prevalence and Impact on Daily Life
PDA is widely recognised in the United Kingdom, particularly in the realms of education, support, and community sector organisations. However, the understanding of the condition is still cursory, primarily because of the absence of explanatory research and the use of synonyms. There are clinical systematic reviews and anecdotal awareness that continue to illustrate the absence of clinical standards.
Certain demand-avoidance behaviour patterns present in PDA children and adults affect school attendance, family routines, and quality of life in general. Families experience pressures that make them feel the need to implement some of the traditional approaches that may escalate rather than mitigate the distress. Support tailored to the PDA characteristics—low-arousal strategies, collaborative communication, and flexible expectations—may significantly improve distress levels.

Support Strategies for PDA
Supporting a person who has a PDA profile requires approaches that are significantly different from traditional behaviour strategies. Since PDA is caused by a fear of threats, anxiety, and a need for autonomy, the main support should be on the improvement of the relationships and emotional safety.
Building Trust Through Relationship-Based Approaches
PDA support is fundamentally anchored on a close, harmonious relationship. Rather than focusing on control and compliance, parents and teachers prioritise engagement and partnership, which helps to alleviate the feeling of external control that so often drives the avoidance.
An approach characterised by low-arousal remains optimal. This involves maintaining a tone of voice, body language, and expectations that are calm and non-confrontational. When a child or adult senses safety rather than pressure, their nervous system become more receptive to engagement.
Using Flexible, Adaptive Communication
For demand-avoidant individuals, phrasing matters. Direct requests can feel like threats, so adapting communication often prevents distress. Examples include:
- Offering choices instead of commands
- Framing tasks as shared activities (“Shall we do this together?”)
- Depersonalising requests (“The bin needs emptying” instead of “You need to empty it”)
These strategies reduce perceived pressure and maintain the person’s autonomy.
Indirect praise is also helpful. Instead of spotlighting behaviour (“Well done for tidying”), focusing on outcomes (“The room feels much calmer now”) avoids triggering shame or expectation.
Supporting Emotional and Sensory Regulation
Many people with a PDA profile have a neurodivergent nervous system prone to sensory overload and emotional lability. Regulation tools can make everyday demands feel more manageable. Helpful approaches include:
- Noise-reduction headphones
- Weighted blankets
- Sensory corners or low-stimulation spaces
- Visual timers
- Movement breaks
Practical Daily Strategies and Adaptive Skills
In daily life, flexible routines work better than rigid schedules. PDA individuals often benefit from:
- Predictable transitions
- Collaborative planning
- Visual schedules with built-in freedom
- Humour and playful engagement to ease tension
These alternative approaches contrast with traditional strategies, which may unintentionally escalate distress by increasing demands or focusing on compliance.
Distraction techniques such as changing the subject, imaginative scenarios, or redirecting attention can assist a person in navigating around avoidance to get through the work.
When to Seek Professional or Community Support
Many families benefit from the help of child psychologists, occupational therapists, and neurodevelopmental experts familiar with the unique autistic profile of PDA. Support from the community, including peer-led support groups and the bigger PDA community, can provide advice, validation, and empathy through shared experiences.
When the behavioural profile brings challenges to school attendance, affects emotional well-being, or disrupts family relationships, seeking tiered support through support teams can mitigate the risk of escalating challenges and to ensure each individual feels seen, heard, and supported.
Frequently Asked Questions About PDA
Is PDA an official diagnosis?
No. PDA does not appear in the DSM-5 or ICD-11. Instead, clinicians understand it as a distinct profile within autism or as a behavioural pattern that may overlap with anxiety, ADHD, or other neurodevelopmental conditions.
Is PDA the same as Oppositional Defiant Disorder (ODD)?
No. While both involve avoidance and resistance, PDA is driven by anxiety and perceived loss of control, whereas ODD is defined by persistent anger, irritability, and defiance. PDA individuals often use social strategies and experience demand avoidance as a stress response rather than intentional opposition.
Can PDA occur without autism?
Most research places PDA within the autism spectrum, but some non-autistic children display PDA-like traits due to anxiety, trauma, or unmet support needs.
How can families support PDA individuals?
Support strategies should prioritise low-arousal approaches, collaborative communication, and flexible expectations.
When should further assessment be sought?
If demand avoidance significantly impacts school attendance, family life, or emotional well-being, it’s time to seek professional help.
Pathological Demand Avoidance: Conclusion
Understanding pathological demand avoidance can help families, professionals, and neurodivergent individuals better identify what’s driving extreme demand avoidance and what kind of support actually works. If these patterns feel familiar, speaking with a clinician can help you explore whether autism, ADHD, or a related profile is involved.=
You can book a free introductory call with us. We’ll be happy to discuss your concerns and provide guidance on the right next steps.
References:
- Kildahl, A. N., Helverschou, S. B., Rysstad, A. L., Wigaard, E., Hellerud, J. M., Ludvigsen, L. B., & Howlin, P. (2021). Pathological demand avoidance in children and adolescents: A systematic review. Autism, 25(8), 2162–2176. https://doi.org/10.1177/13623613211034382
- Moore, A. (2020). Pathological demand avoidance: What and who are being pathologised and in whose interests? Global Studies of Childhood, 10(1), 39–52. https://doi.org/10.1177/2043610619890070
You Might Also Like
Contact Us
We’re here to answer any questions you might have.
Get in Touch
Opening Hours
Contact Form
We’re here to help. Reach out and we’ll get back to you within 24 hours (Monday – Friday).



