
If your child has difficulty focusing, experiences mood swings, or can’t stay in one place long enough to complete an activity, you may already be considering checking if these are signs of ADHD. Some parents notice patterns as early as preschool, long before a teacher expresses concern. The value in early pattern recognition is to be able to help children get the support they need as early as possible.
Exploring professional evaluation options is one way to acquire proper support for your child. You can book a free intro call with us, and we’ll be happy to check in with you to see if your child needs help from our ADHD assessment specialists to conduct a thorough and accurate diagnosis designed to put your child’s needs first.
This article outlines what you can use as an ADHD symptoms in children checklist for parents and teachers, along with a description of traits to look for at home and in the classroom.
Key Symptoms of ADHD in Children
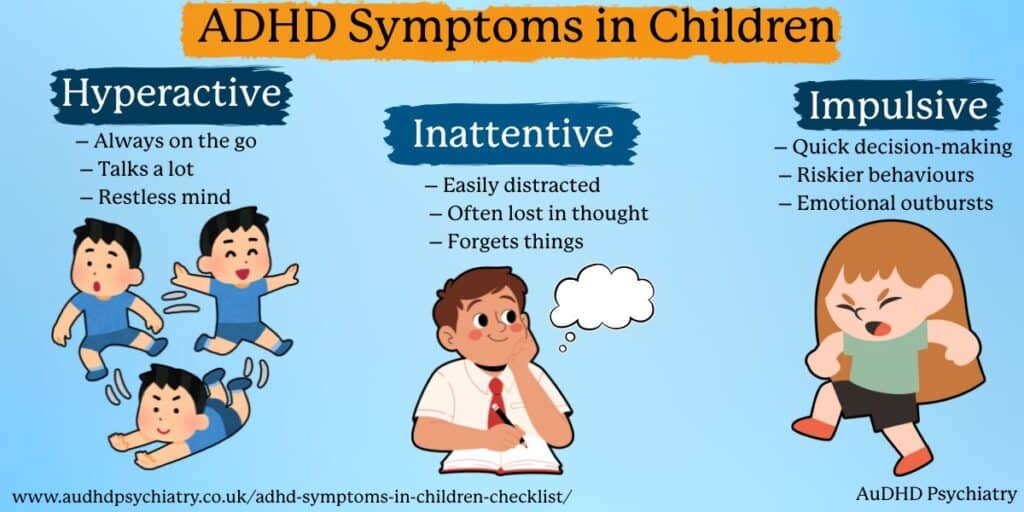
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder that affects areas of the brain responsible for self-control, activity level, and attention. Children can show a wide range of symptoms in everyday tasks, as well as school activities, and regulating their emotions. Let’s discuss how the top ADHD traits show up in children.
Inattention
They may display the following symptoms of inattention.
- They often tend to make careless mistakes in schoolwork.
- They often struggle to follow instructions, even simple ones they understand.
- They tend to lose focus quickly during daily activities.
- They tend to avoid or delay tasks that require sustained attention.
- They often forget about deadlines or where they placed their belongings.
- They tend to zone out or daydream during activities.
- They tend to show signs of distractibility, especially in crowded places.
Such traits are consistent with ADHD, especially among children with a profile of inattentiveness or a combination of types.
Hyperactivity
Hyperactivity is perhaps the most widely known ADHD trait and may include symptoms such as:
- They tend to always move about or display hyperactive behaviors.
- They tend to have difficulties sitting still during lessons or mealtimes.
- They tend to talk excessively and/or interrupt people often.
- They often tend to fidget, tap or show signs of restlessness.
- They often have high energy levels even during moments of quiet play.
Hyperactivity may be more visible when children are expected to sit still and/or follow a routine.
Impulsivity
- Children who display the following symptoms may show a degree of impulsiveness.
- They often tend to act before they think through the consequences of their actions.
- They often tend to grab things, interrupt people, or speak out of turn.
- They tend to have difficulties waiting for their turn to do something.
- They often escalate their emotional responses very quickly.
This is often referred to as hyperactive impulsivity.
Other Areas to Consider
Academic Difficulties
Children may often struggle to focus on the task at hand for long enough to complete it, as well as remember and/or organise their work. For further assistance, refer to ADHD Study Hacks.
Emotional Regulation
The phenomenon of emotional swings and frustrations followed by feelings of difficulty calming down after episodes of excitement or disappointment is common.
Executive Functioning
Children might have difficulty with planning tasks, transitioning between activities, and managing time during transitions.
Daily Routines
The challenges we’ve listed can potentially affect children’s:
- Morning routines
- Hygiene
- Homework
- Bedtime
- Eating and transitioning between meals
- Worsening symptoms of sleep disorders or sleep disturbances.
It’s important to note that some children are more sensitive to noise, touch, textures, or overly bright environments and become overloaded or overwhelmed.
Scannable Checklist (Quick Reference)
If you only have a couple of minutes to research about child ADHD symptoms, see this checklist:
For Parents
- Easily distracted
- Loses items often
- Emotional outbursts
- Difficulty switching tasks
- Appears disorganised
- Struggles with quiet activities
For Teachers
- Struggles with instructions
- Fidgets constantly
- Talks excessively
- Academic inconsistency
- Frequently off-task
- Needs repeated reminders
Child ADHD Symptoms: Girls vs Boys
ADHD manifests in different forms depending on a child’s age and gender. Research has shown that girls are underdiagnosed, and their challenges are often missed. Because of the expectations that accompany the symptoms of ADHD, parents tend to be more concerned when there is visible and overt impulsive and hyperactive behaviour. Girls, on the other hand, have subtle and internal challenges that are often overlooked.
Quiet Inattentive Presentation in Girls
Inattentive symptoms in girls, such as hyperactivity, are more likely to appear in a subtle manner. Rather than a hyperactive child, a teacher may observe a daydreaming or shy girl who seems to be compliant, but is internally having a hard time focusing, organising tasks in a systematic manner, or following through steps in given instructions. These patterns can be mistaken for anxiety or low confidence rather than ADHD.
For these girls, there are no visible challenges. This, however, should not be interpreted as them having no challenges. Apart from the teacher, their classmates and parents may also not be aware of the challenges, which can co-occur or lead to other mental health issues such as anxiety, overwhelm, emotional burnout, and mental health.
Learn more about ADHD without hyperactivity in this article.
Visible Hyperactivity in Boys
Boys tend to express the more typical behaviours associated with ADHD. A behaviour of concern in a child of this age would include running, climbing, interrupting, and/or difficulty remaining seated. This causes teachers and/or child paediatric specialists to refer boys more often and at an earlier stage.
Social Skills Challenges in Both Groups
Boys and girls equally may have problems with reading social cues, joining a group of peers, and/or managing a group conflict. Girls mask confusion, and boys show frustration.
Conditions That Can Look Like ADHD in Children
A lot of children demonstrate behaviours that can resemble ADHD, but the cause can be entirely different. This is why checklists can assist with observations, but cannot substitute for a merited assessment. If the symptoms of your child are ambiguous, AuDHD Psychiatry has designed neurodevelopmental assessments for ADHD, autism, and associated conditions in order to provide the best possible diagnosis. Grab a timeslot for a free intro call, and we’ll be happy to help you with your questions.
Anxiety and Mood Disorders
Due to their worry and anxiety, children are often preoccupied and may come off as if their attention is scattered. They may appear to be restless or as if their attention is being diverted elsewhere, displaying behaviours similar to ADHD.

Autism Traits and Sensory Differences
Children who are autistic may find it difficult to deal with sensory overload, changes, or social interactions. ADHD is also characterised by these features, but is caused by different neurological pathways. See ADHD Burnout for details on emotional overload.
Sleep Disorders
Chronic sleep disorders can result in irritability, difficulty concentrating, poor memory, and sluggish behaviour, which coincide with ADHD.
Oppositional Defiant Disorder (ODD)
Children with oppositional defiant disorder argue, refuse to comply, or challenge limits. They may appear to be inattentive or act with poor impulse control, but their motivations are different, as are their approaches to treatment.
Learning Disabilities
Learning disabilities, such as dyslexia, are characterised by difficulty with reading, memory, and processing speed, which can result in disengagement or avoidance of schoolwork. These behaviours may be similar to ADHD but require different approaches for intervention.
Trauma, Stress, and Environmental Factors
Prior experiences of trauma, stress within the family, or unpredictable environments can result in emotional dysregulation or hyper-vigilance. Hyperactivity and poor concentration often mask these behaviours. Because so many conditions overlap during childhood, a structured assessment is often the safest way to understand the full picture.
Using Your ADHD Symptoms in Children Checklist
Checklists are great starting tools for watching child behaviour, but are not diagnostic. ADHD cannot be diagnosed based on one thing, but clinical judgement, directed rating scales, and observations from multiple environments are required for one to be diagnosed. Nonetheless, checklists aid parents in addressing their concerns before consulting with a professional.
The Utility and Constraints of Checklists
A checklist enables consistent monitoring of a child’s behaviour and is designed to help in spotting certain patterns across days or weeks. Since ADHD behaviour is context-dependent, it’s essential to analyse and compare a child’s home behaviour with their behaviour at school, clubs, or in social gatherings.
Noting Symptoms
Parents can be assisted in documenting:
- Triggers
- Routines that are of help or that aggravate symptoms
- Feedback from teachers
- General sleep patterns
- Responses emotionally
Sharing this record with a child psychologist, GP, or SENCO provides more reliable information during a clinical assessment.
When to Raise Concerns
If the child is having trouble with daily tasks or is having problems with peers, it is a good practice to involve a teacher or a trusted adult as soon as possible. If the symptoms are getting in the way of learning, well-being, or having difficulty with relationships, the next step to take will be to get the child’s ADHD symptoms assessed.
For parents getting ready for their child’s ADHD assessment, the following guides could be helpful:
• How to Get Diagnosed With ADHD
• What to Expect at an ADHD Assessment
More Tools and Assistance
Parents can also check out the routines, trackers, and other helpful resources and tools, which enhance the teamwork of parents, educators, and health professionals.

How to Get for Your Child Diagnosed for ADHD
After reviewing a checklist of symptoms related to ADHD, and seeing persistent patterns that warrant attention, the next step is getting an evaluation conducted by a professional. ADHD cannot be diagnosed by a single form, quiz, or observation; it takes a properly organised assessment that includes clinical tools, interviews, and multi-source feedback.
AuDHD Psychiatry offers well-rounded evaluations for ADHD, autism and AuDHD for children, adolescents, and adults. We use gold-standard tools to ensure that your child has the correct diagnosis and adequate support for all that will follow an assessment. We’ll tell you more about how our process works later. For now, let’s look at the general picture of how kids are assessed for ADHD.
How ADHD Is Diagnosed in Children
The majority of clinicians that make diagnoses use the DSM-5 and other acknowledged standards that define the essential characteristics that fall under inattention, hyperactivity, and impulsivity. The main components of these criteria include:
- Behavioral and rating scales by parents and teachers
- Psychometric evaluations assessing the domains of memory, attention, and problem-solving
- A comprehensive clinical history of development and behavior, including sleep, and academic history
- Referral reports to rule out specific medical conditions, as well as auditory and sleep disturbances
- School questionnaires to gain insight into the child’s behavior in the classroom
- These evaluations allow the diagnostic team to assemble the best possible profile of the child.
NHS Pathway
Most parents begin by contacting the GP, who will listen to the parents’ concerns and record them. The GP will refer the child to the Child and Adolescent Mental Health Service (CAMHS) or to a paediatrician with a specialised interest in neurodevelopmental disorders. The GP will act as a primary healthcare coordinator, and will ensure that the school, home, and medical information flows.
NHS services can take up to years to get your child’s symptoms and reports checked, and so parents often look for other routes as well.
Private ADHD Assessment
Private assessments can be beneficial for families who require more clarity in a timely fashion. With AuDHD psychiatry, your child sees a pediatric ADHD specialist. Private assessments provide the following:
Advantages
- Quicker access
- Extended appointment durations
- Cross-specialty feedback
- Customised advice
Disadvantages
- Increased expense
- Needs communication of results with your GP for medication purposes downstream
If you are unsure of the best way to go, the NHS vs Private ADHD Assessment Guide will provide the important differences.
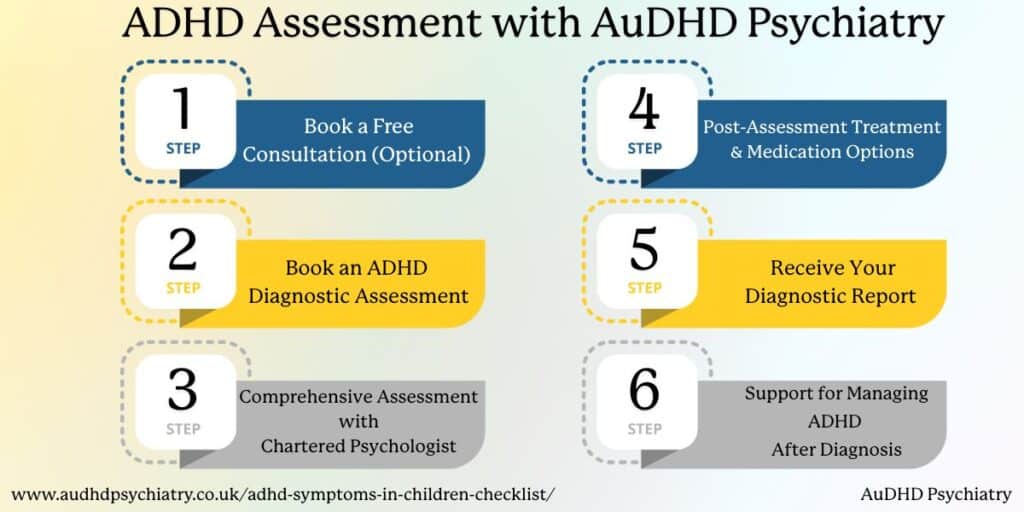
Evaluating ADHD in Children at AuDHD Psychiatry
ADHD is evaluated through a multi-faceted approach rather than a single test. At AuDHD Psychiatry, trained specialists employ the DSM-5 diagnostic criteria in their assessments to capture inattentive, hyperactive-impulsive, and combined presentations, including the more nuanced, subtle patterns in girls, boys, and younger children who may conceal symptoms or behave differently at school and home.
Interviews, behavioural evaluations, and diagnostics are combined in a methodical manner to enable the staff to determine how symptoms manifest in various settings and developmental stages. Each phase has been thoughtfully prepared to ensure clarity, compassion, and ease for families.
Step 1 – Book a Free Consultation (Optional)
This engagement may begin with a complimentary introductory call. You may use this opportunity to describe your concerns, ask questions, and determine if the next step is appropriate at this time (ADHD or autism / AuDHD assessment). A chartered psychiatrist will discuss what to expect and how to get ready.
Step 2 – Book an ADHD Diagnostic Assessment
If you decide to move forward, you will schedule a complete pediatric assessment. We gather background information from you to build a complete clinical picture to address your child’s history, school activities, behaviours, and daily schedule.
Step 3 – Comprehensive Assessment with a Chartered Psychologist
Your clinician conducts an extended interview with individuals to gather data on multiple systems, including symptoms, executive functioning, emotional regulation, and potential comorbidities. In the case of minors, information will also be collected from parents, teachers, and other caregivers in order to evaluate behaviour across multiple settings.
Step 4 – Post-Assessment Treatment & Medication Options
Upon completion of the evaluation process, your clinician will review the most pertinent treatment options, including, but not limited to, behavioural approaches, cognitive behavioural therapy, parent training, ADHD coaching, or, when indicated, stimulant or non-stimulant medications.
Step 5 – Obtain Your Diagnostic Report
You will be provided with a comprehensive, clearly articulated summary of your child’s diagnosis, if any, including ADHD, and specific recommendations to optimise functioning in the classroom, home, and other settings.
Step 6 – Support for Managing ADHD After Diagnosis
Our team provides ongoing assistance through psychotherapy, coaching, and individualised support, enabling families to use real-life strategies. We also provide recommendations regarding school support, EHCP submissions, and ongoing support.
Treatment Options for ADHD Medications
After diagnosis, children can benefit from using multiple treatment methods in combination:
- Stimulant medications or other medications for ADHD
- Behavioral Treatment
- Accommodations for School
- Cognitive Behavioral Therapy for Emotional Issues and Organizational Skills
Each of these options might be recommended based on your child’s needs.

Helping Your Child Manage ADHD Symptoms
Structure, emotions, and ADHD-focused tools need to be integrated to support children with ADHD, and this combination needs to be personalised for each child. This is why we offer follow-up recommendations to support children with home, school, and behavior strategies.
Strategies for ADHD Children at Home
Children tend to do better with predictable routines and structured environments, so children do more effectively with:
- Visual Schedules
- Breaking Tasks into Small Steps
- Transition Timers
- Calm Down Areas with Sensory Tools
- Established Morning and Evening Routines
These strategies reduce overwhelm, ease completion of activities, and facilitate movement. Starting difficult tasks can be an issue, and the guide How to Deal With Task Paralysis offers practical strategies for these scenarios.
School-Based Support
Engaging with your child’s class teacher and/or SENCO can be invaluable. The school can provide:
- Direct and uncomplicated instruction
- Increased wait time
- Alterations of seating arrangements
- Facilitation of breaks during class
- Provision of special educational needs (SEN) support
- Provision of individual positive behaviour support plans
- Provision of adjusted tasks and/or modified homework
Maintaining consistency between school and home helps your child immensely.
Lifestyle, Health, and Well-being
Daily habits play a large role in managing symptoms. Some examples are:
- Improving sleep hygiene
- Balanced nutrition and lifestyle changes
- Regular physical activity
- Teaching skills for emotional regulation
Mindful breathing, body-based coping strategies, along with using sensory tools, can help address mental health concerns for children who may be feeling overwhelmed.
Additional Support for ADHD Symptoms in Children
Structured training programmes, local support groups, and online communities can be helpful for parents. Coaching, as well as Cognitive Behavioural Therapy, can assist with emotional and organisational difficulties. If symptoms are significantly interfering with a child’s ability to focus, learn, or manage emotions, a treatment plan that includes behavioural therapy and/or medication may be warranted.
ADHD Symptoms in Children: Conclusion
Recognising ADHD symptoms early has a positive impact on children’s self-esteem, emotional well-being, and experience with school. The checklist can help you decide on the next steps, which include monitoring your child’s symptoms, having conversations with teachers about your child, and considering a professional assessment. ADHD can be effectively managed when there is the right support, consistent routines, and a compassionate approach to the child’s needs.
Families seeking customised recommendations on our ADHD services can book a free intro call and consult one of our experts. When ADHD is detected early on and supportive systems and strategies are adopted, evidence-based treatments allow for the academic, social, and emotional success of your child.
References:
Quinn, P. O., & Madhoo, M. (2014). A review of attention-deficit/hyperactivity disorder in women and girls: uncovering this hidden diagnosis. The primary care companion for CNS disorders, 16(3), PCC.13r01596. https://doi.org/10.4088/PCC.13r01596
Felt, B. T., Biermann, B., Christner, J. G., Kochhar, P., & Van Harrison, R. (2014, October 1). Diagnosis and management of ADHD in children. AAFP. https://www.aafp.org/pubs/afp/issues/2014/1001/p456.html
You Might Also Like
Contact Us
We’re here to answer any questions you might have.
Get in Touch
Opening Hours
Contact Form
We’re here to help. Reach out and we’ll get back to you within 24 hours (Monday – Friday).




Leave a Reply